Mariam Ibáñez使用大规模测序技术来鉴别急性髓系白血病(AML)起源的新型复发性基因突变的情况。
她简述了本研究面临的挑战:“急性髓系白血病的发展与后天造血祖细胞的获得性基因改变的积累相关。由癌症基因图谱进行的一项研究在23个基因中发现复发性基因突变,99%的急性髓系白血病患者携带至少一种基因突变。然而,许多正常染色体组型患者没有携带已经突变的驱动基因,这些驱动基因与白血病生成的起源和发展相关。”她补充说,“尽管我们取得了进步,但我们继续以诊断急性髓系白血病的三个分子标记改变为基础。因为病人不携带这些突变基因,所以白血病的发病机制是未知的。”因此,本研究的目的是为了确定患者体内新驱动突变基因正常染色体组型。
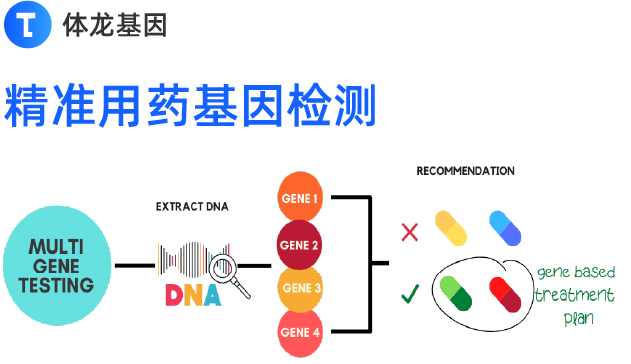
研究组为了找到问题使用了大规模测序技术,分析了近一百个病人体内的一百个基因。早期结果确实显示在这些患者中新基因突变携带强大的潜能可参与急性髓系白血病的发病机理。
此外,通过分析相互作用组(蛋白质之间的交互作用),他们已经能够制出一种计算机模型,该模型可以模拟这种类型白血病的白血病细胞的改变:“在这个模型中,我们可通过物理相互作用,监管,功能和改变细胞路线来分组改变发现。”研究组还没有测试针对现实模型的计算机方法。
这个想法是为了深化白血病生成机制,通过这样做,可以优化治疗急性髓系白血病患者选择:“有了更多的信息我们就能够开发更有效的方法来治疗患者,该方法可靶向急性髓系白血病中的特定分子。”
生物谷相关阅读:
Mariam Ibáñez, lecturer at Universidad Cardenal Herrera CEU (CEU Cardenal Herrera University, UCH-CEU) and biologist at “La Fe” Hospital in Valencia used massive sequencing techniques to identify new recurrent genes mutations involved in the origin of acute myelogenous leukemia (AML).
She outlines the challenge faced by this study: “The development of AML is associated with the accumulation of acquired genetic alterations in hematopoietic progenitor cells. A study performed by the Cancer Genome Atlas discovered recurrent mutations in 23 genes, with 99% of AML patients carrying at least one of these mutations. However, many patients with normal karyotype carry no mutations in any of these recognised driver genes associated with the origination and development of AML (leukemogenesis),” she says, adding that “despite all our advances, we continue to base our diagnosis of AML on the presence of alterations in just three molecular markers. For patients who do not carry these mutations, the mechanisms that lead to the onset of leukemia are unknown.” The aim of this study, therefore, was to identify new driver mutations in patients with normal karyotype and none of the three well-established mutations.
The team approached the problem using massive sequencing techniques, analysing nearly a hundred genes in a hundred patients. Early results did indeed reveal new gene mutations with strong potential to be involved in the pathogenesis of AML in these patients.
Furthermore, by analysing the interactome (the interactions between proteins), they have been able to define a computerised model that simulates the alteration of the leukemia cell in this type of leukemia: “In this model, we have grouped the alterations discovered by physical interaction, regulation, function and altered cellular routes.” The team is yet to test this computerized approach against real-life models.
The idea is to deepen existing knowledge on the mechanisms behind leukemogenesis and, by doing so, be able to optimise the treatment options available to AML patients: “With more information, we would be able to develop more efficient treatments for individual patients that target the specific molecules involved in their AML.”
(责任编辑:sgx)